World
Mpox is a global health emergency. Will it cause a lockdown like COVID? Experts say no
Mpox is now considered a global health emergency as cases surge in Central Africa and a new subtype of the virus, which causes severe illness, spreads to multiple countries — prompting concerns about a lockdown over the virus formerly known as monkeypox in the U.S.
Mpox is a highly contagious viral disease, which can cause flu-like symptoms and painful skin lesions. It’s caused by the mpox virus, which spreads through close contact.
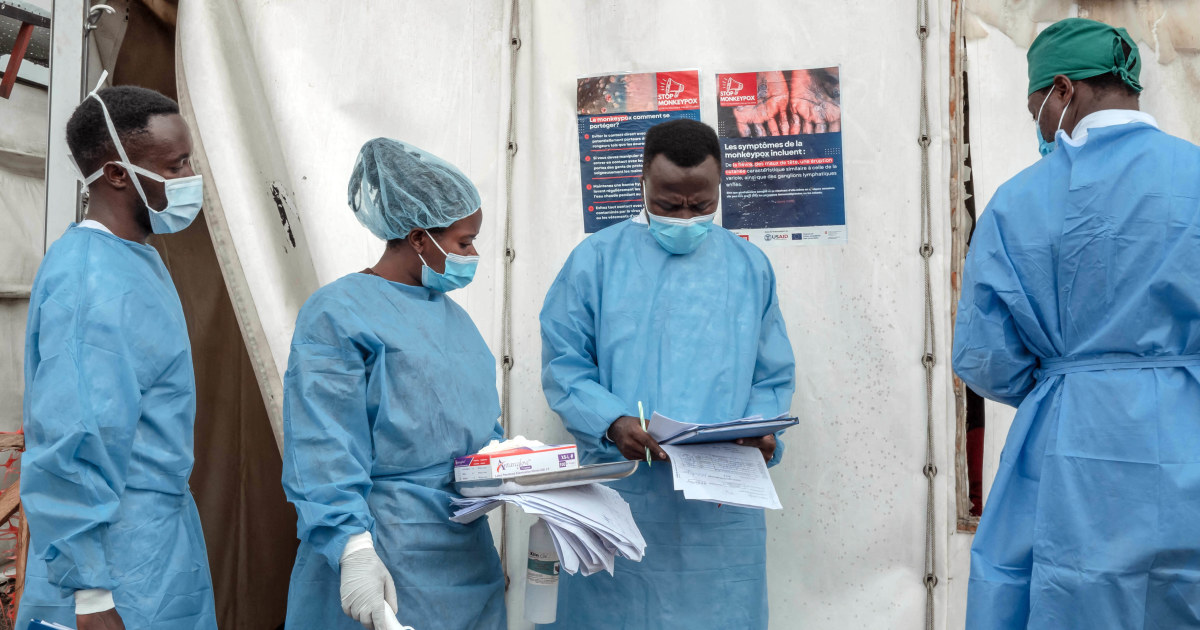
In response to a growing outbreak in the Democratic Republic of Congo and neighboring countries in Africa, the World Health Organization on Aug. 14 declared mpox a public health emergency of international concern (PHEIC), WHO’s highest level of alarm.
This is the second time WHO has declared mpox a PHEIC in two years. The first was in response to a multi-country outbreak in 2022, which sickened nearly 100,000 people, including 32,000 in the U.S., per the U.S. Centers for Disease Control and Prevention.
Although the risk of the current mpox outbreak spreading to people in the U.S. remains very low, experts say, the resurgence of mpox in multiple countries in Africa has raised alarm among scientists. No cases of the new subtype have been reported in the U.S.
Here’s what to know about mpox, where it’s spreading, who is at risk, and symptoms to watch for.
What is mpox?
Mpox is caused by the mpox virus, which is in the same family as the virus that causes smallpox, according to the CDC.
The virus is split into two clades, I and II. Clade I generally causes more severe disease and deaths, with past outbreaks killing up to 10% of those infected, according to the CDC. Clade I mpox is endemic, or regularly found, in Central Africa.
Clade II, which caused the multi-country outbreak in 2022, tends to be the milder form, Dr. Onyema Ogbuagu, an infectious diseases specialist at Yale Medicine, tells TODAY.com.
Clade II is generally more transmissible, but rarely life-threatening. Over 99% of people infected with clade II mpox survive, per the CDC. Clade II mpox is endemic in West Africa.
However, a new subtype of clade I mpox called clade Ib emerged in the DRC in 2023. The new strain, which appears to transmit through sexual networks, has spread rapidly in the DRC and is now being detected in other countries, the WHO said.
Why did WHO declare mpox a global health emergency?
The mpox outbreak in DRC has already spread to at least 12 other countries in the African region, the Africa Centers for Disease Control and Prevention said in a release.
In the past month, more than 100 cases of the newer clade 1b mpox were detected in four countries neighboring the DRC, which have never reported mpox before — Burundi, Kenya, Rwanda and Uganda — officials said.
Shortly before the WHO declaration, the African CDC declared mpox a public health emergency for the continent on Aug. 13.
On Aug. 14, an expert committee advised WHO to consider the upsurge in mpox a global health emergency, with potential to spread further across Africa and potentially outside the continent.
WHO called the emergence of clade Ib mpox and its rapid spread to new countries “especially concerning,” and a “main reason” the agency declared mpox a PHEIC.
“It’s clear that a coordinated international response is needed to stop these outbreaks and save lives,” WHO Chief Dr. Tedros Adhanom Ghebreyesus said in the declaration.
Where is mpox spreading?
At this time, mpox outbreaks have been reported in 13 countries in Africa. The epicenter is in the DRC, Ogbuagu notes.
Clade I mpox has been reported in the DRC for over a decade. Last year, cases surged — the current mpox outbreak is more widespread than any other outbreak in the DRC, according to the CDC.
The number of mpox cases reported in DRC so far in 2024 already exceeds last year’s total, Dr. Daniel Kuritzkes, chief of the division of infectious diseases at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School, tells TODAY.com.
One day after the WHO declaration, Swedish officials confirmed the first case of clade I mpox ever reported outside Africa. The mpox patient in Sweden became infected while traveling in Africa where the outbreak was occurring, officials said in a statement on Aug. 15.
On Aug. 16, the European Centre for Disease Prevention and Control increased the risk level of clade I mpox for the population of Europe from “very low” to “low.”
“Due to the close links between Europe and Africa, we must be prepared for more imported clade I cases,” the agency’s director, Dr. Pamela Rendi-Wagner, said in a statement.
On Aug. 19, the Philippines reported a new case of mpox, Reuters reported. The patient had no travel history outside the Philippines, and officials are awaiting test results to confirm the strain, the Department of Health told Reuters.
One case of clade II mpox was also recently detected in Pakistan, the country’s health ministry told Reuters.
However, there are likely more cases, experts say.
“What we’re seeing is just tip of the iceberg, so it would not be surprising to see more cases outside of DRC and globally. … An infection anywhere is potentially an infection everywhere,” Anne Rimoin, Ph.D., professor of epidemiology at the University of California, Los Angeles, Fielding School of Public Health, tells TODAY.com.
“Whether or not we’ll see widespread cases is really to be determined,” Rimoin adds.
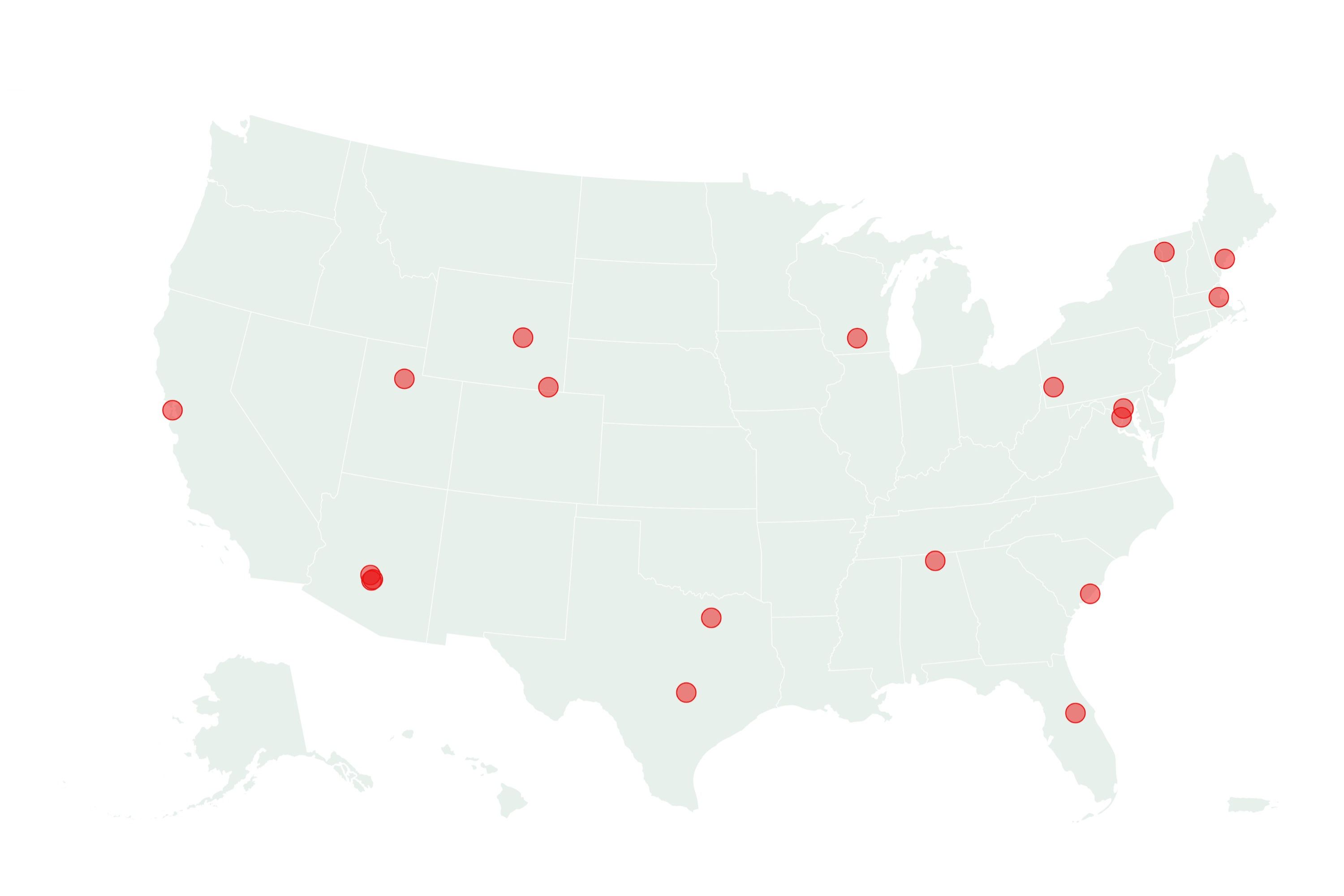
Is there mpox in the U.S.?
Clade II mpox, which caused the 2022 epidemic, is still circulating in the U.S. at low levels, the experts note. “It’s down to single digits or maybe a dozen cases a month,” says Kuritzkes.
There are no known cases of mpox clade I or Ib in the U.S. at this time. “The risk to the general public in the United States from clade I mpox circulating in the DRC is very low,” the U.S. Department of Health and Human Services said in a news release on Aug. 14.
Experts agree that the while it is possible for a person to become infected with clade I mpox in a country where it’s spreading and travel back to the U.S., the chances of this happening are slim.
In a health alert issued on Aug. 7, the CDC stated that the risk of clade I mpox importation into the U.S. was “very low” due to the limited number of travelers and lack of direct commercial flights from the DRC and its neighboring countries to the U.S.
If clade I mpox is imported, “we expect it would cause lower morbidity and mortality in the United States than in the DRC,” the HHS said.
“It’s unlikely that we would see a major outbreak in the U.S.,” says Kuritzkes, adding that mpox is not airborne or spread as easily as respiratory viruses. “It just doesn’t seem very probable because of the type of close contact required.”
Will mpox cause another lockdown?
When asked about the potential for mpox lockdowns, Kuritzkes says “there would be absolutely no reason to take that kind of measure.”
Answering the same question, Rimoin says: “The answer is no. Mpox is not new, like COVID. This is a known virus with tools already available to be able to control it, including vaccines. … We’ve already brought a global outbreak of (mpox) under control in 2022.”
A top WHO official expressed similar sentiments in an Aug. 20 post on X. “Mpox is not the new COVID,” regardless of whether it’s clade I or clade II, Hans Kluge, WHO regional director for Europe, said.
However, experts say increased awareness and surveillance of mpox is important. “Especially in the backdrop of what happened in 2022, I think we need to be not exceedingly worried, but concerned,” says Ogbuagu.
“Clinicians (in the U.S.) are on guard for cases that look like monkeypox, and we will institute the appropriate isolation measures and testing, and we’re ramping up vaccinations for people we perceive to be at risk,” Ogbuagu adds.
How does mpox spread?
Mpox mainly spreads through close contact with an infected person or their lesions, scabs, bodily fluids and respiratory secretions. Transmission can occur during sexual activity but also kissing, hugging, touching and non-intimate face-to-face contact, TODAY.com previously reported.
Mpox can also spread to people through close contact with an infected animal (such as rodents), or direct contact with materials contaminated with the virus, such as clothing or sheets.
The global outbreak in 2022 was primarily sexually transmitted among men who have sex with men and close contacts of infected people, says Ogbuagu.
“The epidemiology in Africa is usually different. Mpox is mostly spread through close contact, without sexual activity,” Ogbuagu adds. Much of the spread has occurred within households, often among children and adolescents, the experts note.
However, the new clade Ib strain, which emerged in DRC, is also being spread through sexual networks, including female sex workers and men who have sex with men, NBC News previously reported.
“(Clade Ib) appears to potentially have characteristics that may possibly make it spread more easily, but it’s not clear at this point,” says Rimoin.
Mpox symptoms
Mpox symptoms typically appear between several days and several weeks after exposure to the virus, per the Cleveland Clinic. These include:
- Rash
- Fever
- Chills
- Fatigue
- Malaise
- Headache
- Muscle aches
- Swollen lymph nodes
These flu-like symptoms often occur before the rash appears, says Ogbuagu. However, some people may only experience a rash.
The mpox rash is typically the most obvious symptom. It goes through several phases before healing, which can take weeks.
The rash often begins as flat, reddish sores which may be painful or itchy. In a few days, these turn into firm, raised bumps, which become fluid-filled blisters and then pustules. These lesions eventually burst and scab over, TODAY.com previously reported.
Lesions usually start on the face and spread to the arms, legs, hands, feet and rest of the body. The sores may also occur on or around the genitals or anus, according to the CDC.
Some people are at higher risk of severe disease, says Kuritzkes. These include people who are immunocompromised, people who have HIV/AIDs, children under the age of 1 and pregnant women.
Mpox treatment
There are no specific treatments or FDA-approved antivirals for mpox. Most healthy people will recover on their own with supportive care, such as pain management and at-home treatment of skin lesions.
However, providers may prescribe other antiviral treatments for more severe cases of mpox or immunocompromised patients, says Kuritzkes. These include tecovirimat (TPOXX) and brincidofovir (Tembexa), which are approved to treat smallpox.
How to prevent mpox
“Prevention is always better than treatment,” says Ogbuagu.
There are several ways to lower your risk of contracting mpox and protect others, according to the CDC. These include:
- Avoid close contact with people who have mpox or a rash that looks like mpox.
- Avoid contact with animals that can carry mpox, such as rodents and primates.
- Get two doses of the mpox vaccine if you’re at risk.
The mpox vaccine is expected to protect against both clades of mpox, the CDC said. It’s recommended for people who have been exposed to mpox or have a higher risk of being exposed.
The CDC has issued a level 2 travel advisory for people traveling to the DRC or neighboring countries, which recommends travelers practice enhanced precautions and seek immediate medical care if they develop a rash.